Differential spectral doppler pattern for the right ventricular outflow tract
DOI:
https://doi.org/10.19137//cienvet202224107Keywords:
echocardiography, doppler, pulmonary artery, spectral tracingAbstract
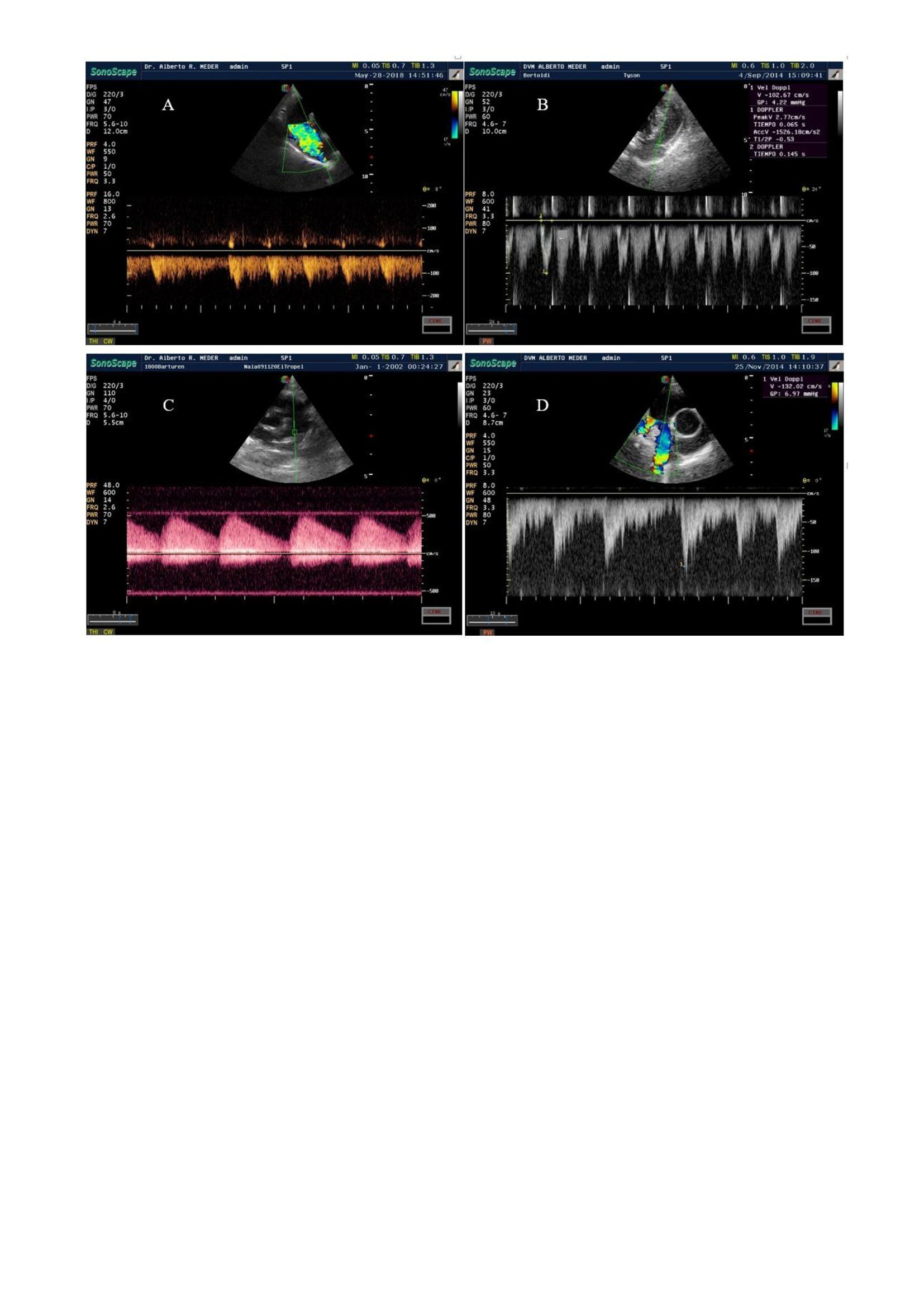
Spectral doppler scanning of the right ventricular outflow tract (RVOT) provides hemodynamic information for the differential diagnosis of heart disease. The flow profile provides data of speed, time, direction and anatomical or functional determination of different changes. The objective of this present work is to analyze the spectral doppler pattern of the right ventricular outflow tract to contribute to the differential diagnosis of heart disease and hemodynamic disorders in pets. The normal ejection spectral trace shows a symmetrical profile, a rounded tip, and tip velocity less than 1.81 m / s (Type I). Pulmonary hypertension, as a consequence of the increased pulmonary vascular resistance, may present a dagger profile, asymmetric, and top speed that is reached within the first third of the spectral trace (Type II). The presence of a gap in the final third of the deceleration curve (flying W), defines the profile as Type III. In stenotic processes top and integral speed time, exceed the normal range and allow to classify the severity of the process. Fixed pulmonary stenosis presents a symmetrical and high-speed profile (> 1.81 m / s). In dynamic obstructions the spectral profile is inverted, reaching the maximum speed at the end of the acceleration curve. When ductus arteriosus is persistent, the flow profile is continuous. Systodiastolic, positive and negative flows, are observed throughout the entire trace. The findings of the spectral doppler scan, by means of the analysis of the flow profile of the right ventricular outflow tract, allow to differentiate pathological processes present, as well as determinate its severity, collaborating in a quick way in the doppler differential diagnosis.
Downloads
References
2. Atkins C, Bonagura J, Ettinger S, Fox P, Gordon S, Haggstrom J, et al. Guidelines for the Diagnosis and Treatment of Canine Chronic Valvular Disease. ACVIM Consensus Statement J. Vet. Intern. Med. 2009 Oct; 23 (6):1142-1150. Doi: 10.1111/j.1939-1676.2009.0392.x
3. Paige CF, Abbott JA, Elvinger F, Pyle RL. Prevalence of cardiomyopathy in apparently healthy cats. J Am Vet Med Assoc. 2009 Jun 1; 234(11):1398-403. doi: 10.2460/
javma.234.11.1398.
4. Wagner T, Fuentes VL, Payne JR, McDermott N, Brodbelt D. Comparison of auscultatory and echocardiographic findings in healthy adult cats. J Vet Cardiol. 2010 Dec; 12(3):171-82. doi: 10.1016/j.jvc.2010.05.003.
5. Payne J R, Brodbelt D C, Fuentes V L. 2015. Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centres (the CatScan study). J Vet Cardiol. 2015; 17:S244-S257 https://doi.org/10.1016/j.jvc.2015.03.008
6. Keene BW, Atkins CE, Bonagura JD, Fox PR, Häggström J, Fuentes VL, Oyama MA, Rush JE, Stepien R, Uechi M. ACVIM consensus guidelines for the diagnosis and treatment of myxomatous mitral valve disease in dogs. J Vet Intern Med. 2019 May; 33(3):1127- 1140. doi: 10.1111/jvim.15488.
7. Fuentes V, Abbott J, Chetboul V, Côté E, Fox PR, Häggström J, Kittleson MD, Schober K, Stern JA. ACVIM consensus statement guidelines for the classification, diagnosis, and management of cardiomyopathies in cats. J Vet Intern Med. 2020 May; 34(3):1062-1077. doi: 10.1111/jvim.15745.
8. Kittleson M D, Kienle R D. Medicina cardiovascular de pequeños animales. 2° Edición. España: Multimédica; 2000.
9. Ettinger S J, Feldman C. Tratado de Medicina Interna Veterinaria. Enfermedades del Perro y el Gato. 6º Ed. Elsevier Saunders; 2007
10. Bonagura J D, Fuentes V F. Echocardiography. En: Mattoon J S, Nyland T G. Small Animal Diagnostic Ultrasound. 3° Ed. Multimédica Ediciones Veterinarias; 2015.
217-332.
11. de Madron E, Chetboul V, Bussadori C. Clinical Echocardiography of the Dog and Cat.. Elsevier Saunders; 2016.
12. Campbell F E. Cardiac Effects of Pulmonary Disease. The Veterinary Clinics of North America: Small Animal Practice. 2007; 37(5):949-962. doi:10.1016/j.
cvsm.2007.05.006
13. Reinero C, Visser LC, Kellihan HB, Masseau I, Rozanski E, Clercx C, Williams K, Abbott J, Borgarelli M, Scansen BA. ACVIM consensus statement guidelines for the diagnosis, classification, treatment, and monitoring of pulmonary hypertension in dogs. J Vet Intern Med. 2020 Mar; 34(2):549-573. doi: 10.1111/jvim.15725.
14. Bonagura J D, Miller M W. Veterinary echocardiography. American Journal Cardiology Ultrasound & Allied Tech. 1989; 6(3):299-264. https://doi.org/
10.1111/j.1540-8175.1989.tb00304.x
15. Boon J A. Ecocardiografía Veterinaria. 2° Edición. España. Multimédica; 2012
16. Chan IP, Weng MC, Hsueh T, Lin YC, Lin SL. Prognostic value of right pulmonary artery distensibility in dogs with pulmonary hypertension. J Vet Sci. 2019 Jul; 20 (4):e34. doi: 10.4142/jvs.2019.20.e34.
17. Lee Y, Choi W, Lee D, Chang J, Kang JH, Choi J, Chang D. Correlation between caudal pulmonary artery diameter to body surface area ratio and echocardiography-estimated systolic pulmonary arterial pressure in dogs. J Vet Sci. 2016 Jun 30;17(2):243-51. doi: 10.4142/jvs.2016.17.2.243.
18. Rhinehart JD, Schober KE, Scansen BA, Yildiz V, Bonagura JD. Effect of Body Position, Exercise, and Sedation on Estimation of Pulmonary Artery Pressure in Dogs with Degenerative Atrioventricular Valve Disease. J Vet Intern Med. 2017 Nov; 31(6):1611- 1621. doi: 10.1111/jvim.14814.
19. Bonagura J D, Miller M W, Darke P G. Doppler Echocardiography. I. Pulsed-wave and Continuous-Wave Examinations. The Veterinary Clinics of North America: Small Animal Practice. 1998; 28 (6):1325-1359 DOI: 10.1016/s0195-5616(98)50126-x
20. Soydan LC, Kellihan HB, Bates ML, Stepien RL, Consigny DW, Bellofiore A, Francois CJ, Chesler NC. Accuracy of Doppler echocardiographic estimates of pulmonary artery pressures in a canine model of pulmonary hypertension. J Vet Cardiol. 2015 Mar; 17(1):13-24. doi: 10.1016/j.jvc.2014.10.004.
21. Jonhson L. Diagnosis of Pulmonary Hypertension.Vet Clin Northam Small Anim. pract. 1999; 14 (4):231-236 DOI: 10.1016/S1096-2867(99)80016-4.
22. Visser LC, Im MK, Johnson LR, Stern JA. Diagnostic Value of Right Pulmonary Artery Distensibility Index in Dogs with Pulmonary Hypertension: Comparison with Doppler Echocardiographic Estimates of Pulmonary Arterial Pressure. J Vet Intern Med. 2016 Mar-Apr;30(2):543-52. doi: 10.1111/jvim.13911. Epub 2016 Feb 19. PMID: 26893108; PMCID:
23. Kirberger R M, Bland-vanden Berg P, Darazs B. Doppler echocardiography in the normal dog: Part I, Velocity findings and flow patterns. Vet. Radiol. Ultrasound. 1992; 33 (6):370-379. https://doi.org/10.1111/j.1740-8261.1992.tb00162.x
24. Brown DJ, Knight DH, King RR. Use of pulsed-wave Doppler echocardiography to determine aortic and pulmonary velocity and flow variables in clinically normal dogs. Am J Vet Res. 1991 Apr; 52(4):543-50. https://pubmed.ncbi.nlm.nih.gov/2053722/
25. Yuill CD, O’Grady MR. Doppler-derived velocity of blood flow across the cardiac valves in the normal dog. Can J Vet Res. 1991 Apr;55(2):185-92. PMID: 1884300
26. Gaber C. Doppler echocardiography. Probl Vet Med. 1991 Dec; 3(4):479-99. https:// pubmed.ncbi.nlm.nih.gov/1802267/
27. Vezzosi T, Domenech O, Iacona M, Marchesotti F, Zini E, Venco L, Tognetti R. Echocardiographic Evaluation of the Right Atrial Area Index in Dogs With Pulmonary Hypertension. J. Vet. Intern. Med . 2018; 32 (1):42-47 DOI:10.1111/jvim.15035.
28. Serres FJ, Chetboul V, Tissier R, Carlos Sampedrano C, Gouni V, Nicolle AP, Pouchelon JL. Doppler echocardiography-derived evidence of pulmonary arterial hypertension in dogs with degenerative mitral valve disease: 86 cases (2001-2005). J Am Vet Med Assoc. 2006 Dec 1; 229(11):1772-8. doi: 10.2460/javma.229.11.1772
29. Paige CF, Abbott JA, Pyle RL. Systolic anterior motion of the mitral valve associated with right ventricular systolic hypertension in 9 dogs. J Vet Cardiol. 2007 May; 9(1):9- 14. doi: 10.1016/j.jvc.2006.08.003.
30. Venco L, Mihaylova L, Boon JA. Right Pulmonary Artery Distensibility Index (RPAD Index). A field study of an echocardiographic method to detect early development of pulmonary hypertension and its severity even in the absence of regurgitant jets for Doppler evaluation in heartworm-infected dogs. Vet Parasitol. 2014 Nov 15; 206(1- 2):60-6. doi: 10.1016/j.vetpar.2014.08.016. Epub 2014 Sep 1
31. Abbott JA, Gentile-Solomon JM. Measurement Variation and Repeatability of Echocardiographic Variables Used to Estimate Pulmonary Artery Pressure in Dogs. J Vet Intern Med. 2017 Nov; 31(6):1622-1628. doi: 10.1111/jvim.14846.
32. Borgarelli M, Abbott J, Braz-Ruivo L, Chiavegato D, Crosara S, Lamb K, Ljungvall I, Poggi M, Santilli RA, Haggstrom J. Prevalence and prognostic importance of pulmonary hypertension in dogs with myxomatous mitral valve disease. J Vet Intern Med. 2015 Mar-Apr; 29(2):569-74. doi: 10.1111/jvim.12564.
33. Schober KE, Baade H. Doppler echocardiographic prediction of pulmonary hypertension in West Highland white terriers with chronic pulmonary disease. J Vet Intern Med. 2006 Jul-Aug; 20(4):912-20. doi: 10.1892/0891-6640(2006)20[912:depoph]2.0.co;2.
34. Paradies P, Spagnolo PP, Amato ME, Pulpito D, Sasanelli M. Doppler echocardiographic evidence of pulmonary hypertension in dogs: a retrospective clinical investigation. Vet Res Commun. 2014 Mar; 38(1):63-71. doi: 10.1007/s11259-013-9588-4
35. Akabane R, Shimano S, Sakatani A, Ogawa M, Nagakawa M, Miyakawa H, Miyagawa Y, Takemura N. Relationship between right heart echocardiographic parameters and invasive pulmonary artery pressures in canine models of chronic embolic pulmonary hypertension. J Vet Med Sci. 2019 Oct 24; 81(10):1485-1491. doi: 10.1292/ jvms.19-0350.
36. Johnson LR, Stern JA. Clinical features and outcome in 25 dogs with respiratory-associated pulmonary hypertension treated with sildenafil. J Vet Intern Med. 2020 Jan; 34(1):65-73. doi: 10.1111/jvim.15679.
37. Uehara Y. An attempt to estimate the pulmonary artery pressure in dogs by means of pulsed Doppler echocardiography. J. Vet. Sci. 1993; 55(2):307–312 doi: 10.1292/ jvms.55.307
38. Ristic JM, Marin CJ, Baines EA, Herrtage ME. Congenital Pulmonic Stenosis a Retrospective study of 24 cases seen between 1990-1999. J Vet Cardiol. 2001 Nov; 3(2):13- 9. doi: 10.1016/S1760-2734(06)70015-7.
39. Tobias AH, Stauthammer CD. Minimally invasive per-catheter occlusion and dilation procedures for congenital cardiovascular abnormalities in dogs. Vet Clin North Am Small Anim Pract. 2010 Jul; 40(4):581-603. doi: 10.1016/j.cvsm.2010.03.009.
40. Francis A J, Johnson M J, Culshaw G C, Corcoran B M, Martin M W S, French A T. Outcome in 55 dogs with pulmonic stenosis that did not undergo balloon valvuloplasty or surgery. J.Small Anim. Pract.. 2011; 52(6):282–288 https://doi. org/10.1111/j.1748-5827.2011.01059.x
41. Johnson M S, Martin M, Edwards D, French A, Henley W. Pulmonic stenosis in dogs: balloon dilation improves clinical outcome. J.Vet. Intern. Med. 2004; 18 (5):656-62 doi: 10.1892/0891-6640(2004)18<656:psidbd>2.0.co;2.
42. Loureiro J, Smith S, Fonfara S, Swift S, James R, Dukes-McEwan J. Canine dynamic left ventricular outflow tract obstruction: assessment of myocardial function and clinical outcome. J Small Anim Pract. 2008 Nov; 49(11):578-86. doi: 10.1111/j.1748-5827.2008.00623.x.
Downloads
Published
How to Cite
Issue
Section
License
Al momento de enviar sus contribuciones, los colaboradores deberán declarar , de manera fehaciente, que poseen el permiso del archivo o repositorio donde se obtuvieron los documentos que se anexan al trabajo, cualquiera sea su formato (manuscritos inéditos, imágenes, archivos audiovisuales, etc.), permiso que los autoriza a publicarlos y reproducirlos, liberando a la revista y sus editores de toda responsabilidad o reclamo de terceros , los autores deben adherir a la licencia Creative Commons denominada “Atribución - No Comercial CC BY-NC-SA”, mediante la cual el autor permite copiar, reproducir, distribuir, comunicar públicamente la obra y generar obras derivadas, siempre y cuando se cite y reconozca al autor original. No se permite, sin embargo, utilizar la obra con fines comerciales.






4.png)


7.png)



